Understanding the differences between Crohn’s disease and celiac disease is essential, as these conditions affect the digestive system in distinct ways. Both conditions can cause discomfort, but their origins, symptoms, and treatments vary significantly. Let’s explore these key differences:
Symptoms:
Crohn’s Disease:
Crohn’s disease is a type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. Its inflammation can extend deep into the layers of the bowel tissue.
- Abdominal Pain: Often cramping, especially in the lower right abdomen.
- Diarrhoea: Sometimes, it is accompanied by blood or mucus.
- Fatigue: A sense of constant tiredness due to malabsorption and inflammation.
- Weight Loss: Unintentional weight loss due to nutrient malabsorption.
- Fever: Low-grade fevers may accompany inflammation.
- Mouth Sores: Ulcers may form in the mouth.
- Fistulas: In severe cases, abnormal connections may form between different parts of the intestines or between the intestines and other organs.
- Joint Pain: Some individuals may experience joint inflammation.
Celiac Disease:
Celiac disease is an autoimmune disorder where the ingestion of gluten (a protein found in wheat, barley, and rye) leads to damage in the small intestine.
- Bloating and Gas: Common after consuming gluten.
- Diarrhea or Constipation: Both can occur, often due to malabsorption of nutrients.
- Abdominal Pain: Similar to Crohn’s but triggered specifically by gluten consumption.
- Weight Loss or Inability to Gain Weight: Malabsorption of nutrients leads to weight issues.
- Fatigue: This is a result of nutrient deficiencies, especially iron and vitamin B12.
- Skin Rash: Dermatitis herpetiformis, a blistering rash, may appear in some cases.
- Mouth Ulcers: Similar to Crohn’s, but typically linked to gluten exposure.
- Bone or Joint Pain: Often due to calcium and vitamin D malabsorption, leading to conditions like osteoporosis.
Causes:
- Crohn’s Disease: The exact cause is unknown, but it’s thought to be a combination of genetics, immune system issues, and environmental factors. Unlike celiac disease, Crohn’s is not triggered by a specific food.
- Celiac Disease: Triggered by the ingestion of gluten, which causes the immune system to attack the lining of the small intestine, leading to damage over time.
Diagnosis:
Crohn’s Disease:
- Colonoscopy: Used to view the entire colon and take biopsies.
- Imaging Tests: Such as CT scans or MRIs to detect inflammation in the digestive tract.
- Blood Tests: To check for inflammation and anaemia.
- Celiac Disease:
- Blood Tests: Used to detect specific antibodies related to celiac disease (e.g., tissue transglutaminase antibody test).
- Biopsy of the Small Intestine: Confirmatory test after blood tests, often done via endoscopy.
Treatment:
Crohn’s Disease:
Medications:
- Anti-inflammatory Drugs: Such as corticosteroids and aminosalicylates.
- Immunosuppressants: To reduce the immune response causing inflammation.
- Biologics: Target specific proteins involved in the inflammation process.
- Antibiotics: To treat infections that might develop due to fistulas or abscesses.
Dietary Adjustments:
- Low-Residue Diet: Reduces fiber to lessen the frequency of bowel movements.
- Nutritional Supplements: Due to malabsorption of vitamins and minerals.
- Surgery: In severe cases, surgery may be required to remove damaged portions of the intestine.
Celiac Disease:
- Strict Gluten-Free Diet: The cornerstone of celiac treatment. Complete elimination of gluten from the diet is necessary to allow the small intestine to heal.
- Supplements: Depending on the damage to the small intestine, supplements like iron, calcium, vitamin D, and B12 may be necessary to address deficiencies.
Symptom Relief:
- Anti-inflammatory Medications: To manage symptoms during the initial gluten-free transition.
- Enzyme Supplements: It may help with digestion until the gut heals fully.
- Prognosis and Management:
Crohn’s Disease:
It’s a chronic condition, and while there’s no cure, symptoms can often be managed with a combination of medication, lifestyle changes, and possibly surgery. Flares can occur, and ongoing monitoring by healthcare providers is essential.
Celiac Disease:
If diagnosed and treated early with a strict gluten-free diet, most people with celiac disease can live healthy, symptom-free lives. However, accidental gluten exposure can cause setbacks.
Key Differences at a Glance:
| Feature | Crohn’s Disease | Celiac Disease |
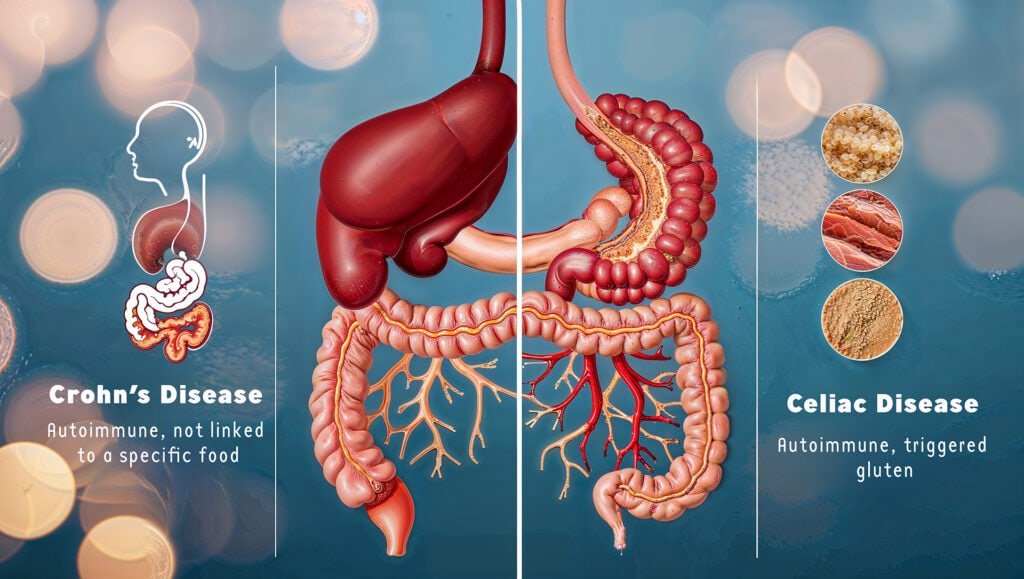
| Cause | Autoimmune, not linked to a specific food | Autoimmune, triggered by gluten |
| Area Affected | Can affect any part of the GI tract | It can affect any part of the GI tract |
| Symptoms Triggered By | Not triggered by food, flares can occur unpredictably | Triggered by the ingestion of gluten |
| Main Treatment | Medications, surgery, and dietary adjustments | Gluten-free diet |
| Prognosis | No cure, but symptoms can be managed | It primarily affects the small intestine |
Both conditions require careful management and lifestyle changes, but many individuals can achieve a good quality of life with the right approach.
Wishing you balance and health on your wellness journey.
Warm regards,
Dr. Deepthi Niranjan
Indus Valley Ayurvedic Centre and Wellness Resort, India
- BA in Ayurvedic Medicine and Surgery (Kayachikitsa & Panchakarma)
- Rajiv Gandhi University of Health Sciences (RGUHS)
- Graduated in 2003
- Expertise in Ayurvedic diagnosis, Panchakarma detoxification therapies, and holistic wellness practices.Indus Valley Ayurvedic Centre (IVAC)

